
The lifetime prevalence of eating disorders, including anorexia nervosa, bulimia nervosa, and binge eating disorder, hovers just under 5 percent. Individuals with eating disorders are likely to experience sleep issues, particularly difficulty falling asleep, frequent nighttime awakenings, and short sleep overall. In many cases, these issues share a directional relationship: the more severe their eating disorder is, the worse the individual sleeps.
Researchers hypothesize that increased stress levels and hormonal imbalances, due to the strain of food restriction, weight fluctuation, and disturbed sleep, may exacerbate symptoms of both the eating disorder and related sleep problems. Additionally, comorbid mental health issues like depression may contribute to and intensify symptoms.
Eating Disorders and Sleep
Sleep Disturbance and Eating Disorders
Eating disorders affect people of all genders, ages, and ethnic groups. About 4.5 percent of adults may develop an eating disorder at some point during their life times, including anorexia nervosa, bulimia nervosa, and binge eating disorder.
Eating disorders rarely exist in isolation. Often, they are accompanied by sleep problems such as insomnia and disrupted sleep. For example, one study found that insomnia (difficulty falling and staying asleep) is twice as common among female patients with anorexia or bulimia than women in the general population.
Insomnia itself is associated with an increased risk of eating disorders, and eating disorders are associated with increased instances of insomnia and disrupted sleep. Problematically, a lack of adequate sleep can worsen symptoms of eating disorders, and cause comorbidities like depression or anxiety.
Correlations Between Eating Disorders and Insomnia, Sleep Apnea, and Impaired Daytime Functioning
In the Netherlands, researchers observed the body mass index (BMI), eating disorders, sleep disorders, and daytime functioning among a group of 574 young adults between ages 18 and 35. Of the group, about 12 percent screened positive for an eating disorder. When compared to the participants without eating disorders, these individuals were significantly more likely to have sleep apnea, insomnia, and imapired daytime functioning.
In the charts below, ESP represents the participants’ average scores on the Eating Disorder Screen for Primary Care.
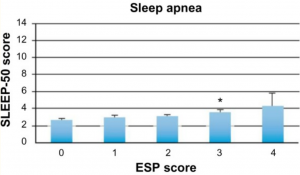
Sleep apnea is a sleep-related eating disorder where the individual momentarily stops breathing during sleep, resulting in a gasping or choking sound that disrupts their sleep cycle, whether they wake up or remain subsconscious. Sleep apnea has been linked to depression, obesity, diabetes, and a three times increased risk of death.
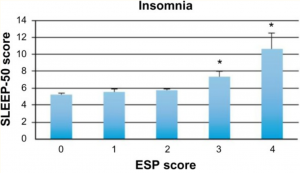
Insomnia describes a chronic difficulty of falling or staying asleep. Temporary insomnia affects about 15 to 20 percent of the population, and usually only lasts a few days to weeks. Chronic insomnia describes a more persistent, severe form of the disorder and lasts for months or more. It affects about 10 percent of the general population.

Impaired daytime functioning describes the effects of sleep deprivation, like that caused by sleep apnea or insomnia. Even one night of sleep deprivation can result in impaired cognitive performance, poor mood or irritability, impaired judgment, delayed reaction times, and reduced wellbeing.

Find out more




